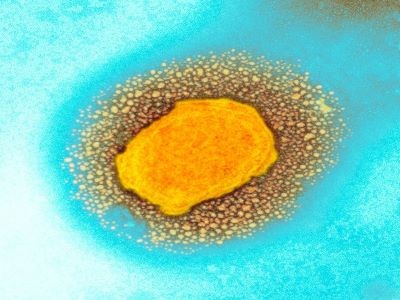
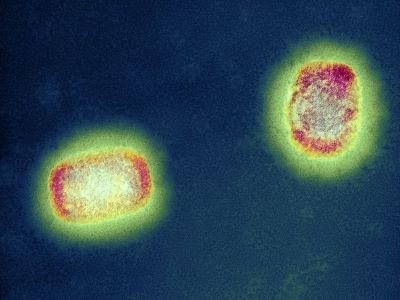
After monkeypox cases exploded last month in countries such as Portugal, Spain and the United Kingdom — where outbreaks don’t usually occur — a rapid, global response followed, including the distribution of vaccines in some countries. But monkeypox outbreaks have been occurring in parts of Central and West Africa for years, leaving African researchers there disheartened that such resources have not been made available in their countries, where the disease’s toll has been highest. They point out that they have long been warning of the potential for the monkeypox virus, which has been behaving in new ways, to spread more widely.
So far this year, there have been more than 3,000 confirmed monkeypox cases in countries beyond Central and West Africa, but no deaths have been reported. In Africa, however, health officials have reported more than 70 deaths that they suspect were caused by monkeypox. This is probably an undercount because of limited testing and surveillance capacity, says Dimie Ogoina, an infectious-disease physician at Niger Delta University in Amassoma, Nigeria.
Although he is frustrated by monkeypox having been largely ignored by Western nations until now, Ogoina worries that the current global outbreaks still won’t improve the situation for Africa. “If we don’t draw the attention of the world for this, a lot of the solutions will address the problem in Europe, but not in Africa,” he says.
Experience with outbreaks
Before this year, only a handful of monkeypox cases had been observed outside Africa; these were linked to the importation of animals from the continent or to travellers who had visited. The largest of these outbreaks was a short-lived one in the United States in 2003, which stemmed from imported animals and made more than 70 people ill.
Meanwhile, some African nations have been dealing with monkeypox outbreaks ever since scientists identified the first human case in the Democratic Republic of the Congo (DRC) in 1970. Although researchers still don’t know precisely which animals naturally harbour the virus, they do know that it circulates among many species of rodent and can transmit from animals to humans. A significant outbreak began in Nigeria in 2017, with more than 200 confirmed and 500 suspected cases of monkeypox. Over the past decade, the DRC has seen thousands of suspected cases, as well as hundreds of suspected deaths. In Central Africa, the strain of monkeypox virus that has infected people is more virulent, with a mortality rate of about 10%.
For Adesola Yinka-Ogunleye, an epidemiologist at the Nigeria Centre for Disease Control in Abuja, the current global outbreaks have brought on a certain sense of déjà vu. Before the 2017 Nigeria outbreak, the virus seemed to be confined to rural areas, where hunters would come into contact with animals. It would make its presence known with a fever and distinctive fluid-filled ‘pox’ lesions on the face, hands and feet. After 2017, she and other epidemiologists warned1 that the virus was spreading in an unfamiliar way: it was appearing in urban settings, and infected people sometimes had genital lesions, suggesting that the virus might spread through sexual contact. With the virus now proliferating in Western cities through what seems to be close contact with sexual partners, “the world is paying the price for not having responded adequately” in 2017, she says.
Lowered immunity
At the same time, researchers have been warning that cases of monkeypox in sub-Saharan Africa have been rising for years. In part, this is because countries stopped giving people vaccines against smallpox, which is caused by variola, a virus that is closely related to the one that causes monkeypox. Smallpox was eradicated in 1980 and vaccination was halted, meaning that the percentage of the population vulnerable to it — and thus to monkeypox — has been growing (see ‘Monkeypox cases rising in Africa’).
Monkeypox cases rising in Africa
|
Decade |
Confirmed cases caused by the viral strain that emerged in Central Africa |
Confirmed cases caused by the viral strain that emerged in West Africa |
|---|---|---|
|
1970– 79 |
38 |
9 |
|
1980–89 |
355 |
1 |
|
1990–99 |
520 |
0 |
|
2000–09 |
92 10,027 suspected* |
47 |
|
2009–19 |
85 18,788 suspected* |
195 |
Since that time, some nations have maintained national stockpiles of smallpox vaccines because health officials have been worried that laboratories keeping samples of variola might accidentally release it, or that the virus might be weaponized. Countries including Canada, France, the United Kingdom and the United States have been using these stockpiles in a ‘ring vaccination’ strategy to protect close contacts of a person who is infected with the monkeypox virus. Acknowledging that many cases have so far occurred in men who have sex with men (MSM), authorities in several Canadian cities and in the United Kingdom have gone one step further and begun offering the vaccines to their MSM communities.
Steve Ahuka, a virologist at the University of Kinshasa, says these vaccines would be useful to tackle the outbreaks in Africa — but countries there don’t have large stockpiles, and Western nations haven’t donated their shots for use against monkeypox. Both Ahuka and Yinka-Ogunleye say that if they did have vaccines, they would at the very least recommend inoculating front-line health-care workers and laboratory technicians. Other researchers Nature spoke with also said the shots could help to curb monkeypox in Africa if they were given to people with compromised immune systems and those who frequently encounter wildlife.
A lack of investment
Some health officials in sub-Saharan Africa worry that they will continue to be left behind, judging by their experience of vaccine inequity during the COVID-19 pandemic. Although case numbers are going up, only 18.4% of people in Africa have been vaccinated against the coronavirus SARS-CoV-2, compared with 74.8% in high-income countries elsewhere.
Member nations of the World Health Organization (WHO) have pledged more than 31 million smallpox-vaccine doses to the agency for smallpox emergencies — but these have never been distributed to Africa for use against monkeypox. Part of the reason, says Rosamund Lewis, the technical lead for monkeypox at the WHO, is that some of the agency’s pledged stockpile is made up of ‘first generation’ vaccines; these can have severe side effects and are not recommended for monkeypox, which is less deadly than smallpox. (Lewis declined to specify the precise composition of the WHO’s pledged stockpile.)
She also cites “regulatory issues”, because some member nations have licensed the vaccines only for use against smallpox, not monkeypox. (Although the vaccines are considered safe and effective for use in people with smallpox infection, they have had limited testing against monkeypox.)
“The investment has perhaps not been what we would want it to be, but it’s not been nothing,” Lewis says of efforts to address monkeypox in Africa. She adds that the WHO has been coordinating with African countries that have monkeypox outbreaks to improve surveillance and diagnostics.
In recent weeks, the WHO has recognized the inequity in the global attention that monkeypox is receiving. On 17 June, the agency announced it would no longer report monkeypox cases and deaths for sub-Saharan Africa and the rest of the world separately, reflecting the “unified response that is needed”. And after researchers published a proposal to change the name of monkeypox viral strains — currently called the West African clade and the Congo Basin clade — WHO director-general Tedros Adhanom Ghebreyesus came out in support of the changes, to reduce stigma. He promised to “make announcements about the new names as soon as possible”.
Yet even if sub-Saharan African nations procure vaccines, inoculation alone will not eradicate monkeypox, says Oyewale Tomori, an independent virologist in Ibadan, Nigeria. He cautions that vaccination is only effective if health officials understand the local epidemiology of the pathogen — and there are still many questions about how isolated cases of the disease have continued to pop up all over the affected countries in sub-Saharan Africa. He recommends supporting research to investigate the animal reservoir of monkeypox so that health officials can devise more precise measures to curb the spread of the virus. “Without addressing the fundamental issues, you’ll end up using all your vaccines toward monkeypox,” he says, instead of dealing with the source of the problem — contact between wildlife and humans.
Equally important are strategies to speed up testing for monkeypox, because the faster that a case can be confirmed, the sooner that public-health officials can begin containment countermeasures, Ogoina says. These advances can’t come soon enough for sub-Saharan Africa, he adds. “Isolated solutions that fix the problem for developed countries alone and leave out developing countries will lead us through the same cycle again,” he warns, pointing to past outbreaks where a pathogen continues to re-emerge. “It’s just a matter of time.”
"world" - Google News
June 23, 2022 at 10:57PM
https://ift.tt/UNLtWEY
Monkeypox in Africa: the science the world ignored - Nature.com
"world" - Google News
https://ift.tt/K5veU7g
https://ift.tt/vMjRlHU
Bagikan Berita Ini

















0 Response to "Monkeypox in Africa: the science the world ignored - Nature.com"
Post a Comment